Other
217 - Trainees' Experience with a Poverty Simulation

Sarah Beck, DDS
Resident
University of Iowa, Iowa City, IA
University of Iowa College of Dentistry
Iowa City, Iowa, United States- TB
Theresa Bechtel, DNP, RN, PCCN, CNE
University of Iowa, College of Nursing
- MM
Michelle R. McQuistan, DDS, MS
University of Iowa, College of Dentistry
- CO
Caitlin Owens, MSW
Iowa's University Center for Excellence on Disabilities
- FQ
Fang Qian, PhD
University of Iowa, College of Dentistry
- KL
Kecia S. Leary, DDS, MS
Clinical Professor
University of Iowa, College of Dentistry
Iowa City, Iowa, United States - HS
Heidi Steinkamp, DDS, MS, PhD
University of Iowa, College of Dentistry
Iowa City, Iowa, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
Purpose: Health disparities disproportionately affect vulnerable populations, particularly the poor and elderly. The purpose of this longitudinal study is to assess shifts in the attitudes of University of Iowa Leadership Education in Neurodevelopmental Disabilities (LEND) students, nursing students, and faculty/ staff regarding treating underserved populations based on an educational model that incorporates a poverty simulation as component of their education.
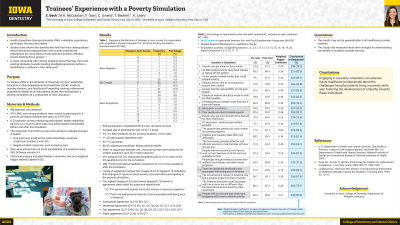
Methods: Four hundred and ten LEND and nursing students were invited to participate in a poverty simulation between the years 2019-2023. A 20-question survey measuring participants’ beliefs regarding poverty on a 5-point Likert scale was administered immediately before and after the simulation. The responses from both surveys were paired to evaluate changes in beliefs. Statistical analysis included Bowker’s symmetry test and weighted Kappa statistic (alpha=0.05).
Results: The study comprised 385 participants who completed both pre- and post-surveys. Shifts in responses between pre- and post-surveys were observed for sixteen questions (P < .05 in each instance). Notably, 201 subjects (52%) responded empathetically to 16 or more of the 20 questions prior to the simulation while 288 (75%) provided empathetic responses to 16 or more questions after the simulation. Levels of agreement ranged from kappa=0.62 to kappa=0.16 indicating that changes of opinions about poverty occurred after participating in the poverty simulation.
Conclusions: Engaging in a poverty simulation can educate future healthcare professionals about the challenges faced by patients living in poverty and foster the development of empathy towards these individuals.
Identify Supporting Agency and Grant Number: Research supported by the University of Iowa, College of Dentistry, Department of Pediatric Dentistry.

.jpg)