Sedation
139 - Sedation Regimen and OSA Screening Influence Post-Sedation Discharge Events

Lydia L. Brett, DMD
PGY-2 Pediatric Resdient
University of Texas Health Science Center-Houston
UTHealth Houston School of Dentistry
Houston, Texas, United States- DD
Deniz N. Dishman, PhD, DNAP, MSN, CRNA
UTHeatlh Cizik School of Nursing, Houston, TX
- BA
Bhavini s. Acharya, BDS, MPH
UTHealth Houston School of Dentistry, Houston, TX
- BC
Brett T. Chiquet, DDS, PhD
UTHealth Houston School of Dentistry, Houston, TX

Brett T. Chiquet, DDS, PhD
Associate Professor
University of Texas Health Science Center-Houston
University of Texas School of Dentistry
Houston, Texas, United States- BA
Bhavini Acharya, BDS, MPH
Associate Professor; Program Director, Pediatric Dentistry Residency
University of Texas Health Science Center-Houston
Houston, Texas, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
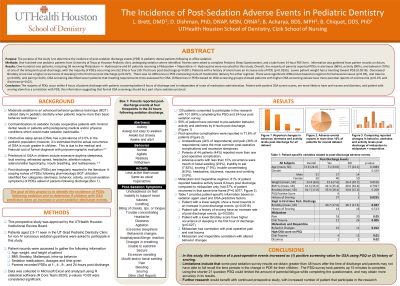
Purpose: The purpose of the study is to quantify the incidence of post-sedation discharge events (PDE) in pediatric dental patients following in-office sedation and determine if PDEs correlate with an obstructive sleep apnea (OSA) screening tool.
Methods: One-hundred-one pediatric patients undergoing sedation were identified. Parents completed the Pediatric Sleep Questionnaire and a take home 24-hour PDE form based on findings from a scoping literature review of PDEs following in-office sedation. Data extracted from electronic dental records included vitals, airway assessment, and sedation regimen. Chi-square and Fisher exact tests were completed; P < .05 were considered significant.
Results: The majority of parents reported PDEs in alertness (96%), activity (90%), and behavior (70%) at one timepoint post-discharge, with the majority of PDEs occurring 1-hour (52%) or 4-hours (30%) post discharge (P < .001). While differences based on regimen in behavioral issues (P=.05), oral trauma (P=.005), and pain (P=.05) were identified, route of medical delivery was not significant (P>.05). OSA screening identified 7 patients that met requirements to be assessed for OSA. Differences in PDEs based on OSA screening showed patients with higher OSA screening values have more parental reports of oral trauma (P=.01) and dizziness (P=.02).
Conclusion: This is the first prospective PDE study evaluating all PDEs previously reported in the literature. Most PDEs occur in the first 4 hours post-discharge, and most patients return to baseline by 8 hours. PDEs are influenced by sedation regimen and positive OSA screening, suggesting that formal OSA screenings should be a part of a pre-sedation protocol.
Identify Supporting Agency and Grant Number:

.jpg)